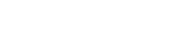
Heart disease is a leading cause of death globally, accounting for millions of deaths each year. It’s a term used to describe a range of conditions that affect the heart, including coronary artery disease, heart failure, and arrhythmias. Heart disease can occur due to several factors such as lifestyle choices, genetic predisposition, or underlying health conditions. Although the condition is common, many people may not know the symptoms and risk factors associated with it.
In this article, we’ll provide you with a comprehensive overview of heart disease, including its common symptoms, risk factors, and treatment options. We’ll explore the lifestyle changes that can help prevent heart disease and the medical interventions that may be necessary to manage the condition. Additionally, we’ll discuss the importance of early detection and seeking medical attention if you experience any of the warning signs. By understanding the complexities of heart disease, you can take proactive steps to protect your heart health and improve your overall well-being.
Types of Heart Disease and Their Symptoms
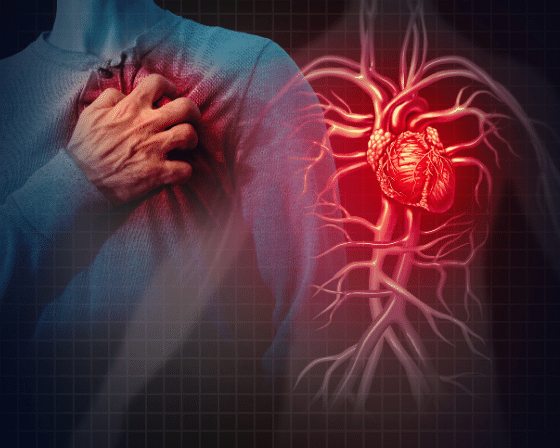
There are several types of heart disease, but the most common type is coronary heart disease, a condition in which the arteries narrow and become blocked over time. Coronary heart disease killed about 366,000 Americans in 2017, according to the CDC.
Symptoms of coronary heart disease include chest pain, shortness of breath or a heart attack. Narrowed arteries can lead to other complications in the body such as stroke. It can also cause irregular or rapid heartbeats.
Other problems affect heart valves or cause the heart to pump inefficiently, which can lead to heart failure. Some individuals are born with certain heart defects that are also associated with heart disease.
Each type of heart disease has its own symptoms. But it’s important to note that some people might not experience any symptoms at all. For example, half the men who suddenly die of coronary heart disease had no previous symptoms, according to the CDC.
Angina
Angina, or chest pain, occurs when the heart doesn’t get enough oxygen, but the symptom doesn’t always mean a person is having a heart attack.
The most common cause of angina is atherosclerosis, or hardening of the arteries. But muscle spasms in the arteries, cold temperatures, strong emotions or other causes may also be to blame.
People may experience angina differently, depending on age, gender and other factors.
Stable angina occurs when the heart is working hard (such as during physical activity), while experiencing emotional stress or after eating a meal, but some people may experience angina while at rest. Angina at rest, or variant angina, is rare.
People may feel symptoms of angina in the chest, upper back, arms, neck, throat, jaw or across the shoulders, but symptoms most often occur in the chest and left arm.
- Aching, burning, squeezing or feelings of fullness or heaviness in the chest
- Indigestion
- Numbness or tingling in the shoulders, arms or wrists
- Shortness of breath
- Squeezing
- Sweating or dizziness
- Tightness
- Pain in the arms, pack, jaw, neck or shoulder accompanying pain in the chest
Stop activity and rest if you feel any of the listed symptoms. Use nitroglycerin tablets or sprays if your provider has prescribed them.
Another type of angina, unstable angina, doesn’t follow a pattern and doesn’t go away with rest or medicine. This is the most dangerous type of angina and is a sign of a possible heart attack.
Heart Attack
A heart attack, or myocardial infarction, happens when blood flow to the heart is blocked. This can damage or even kill parts of the heart muscle. The damage is reversible if blood flow is restored, so individuals who are having a heart attack must get help immediately.
Call 911 immediately and get to the nearest emergency room as quickly as possible if you experience heart attack symptoms.
- Fainting or lightheadedness
- Pain in the chest, shoulders, neck or arms
- Pressure, pain or squeezing in the chest that lasts for more than a few minutes
- Rapid heartbeat
- Shortness of breath
- Sweating
- Vomiting or nausea
- Weakness
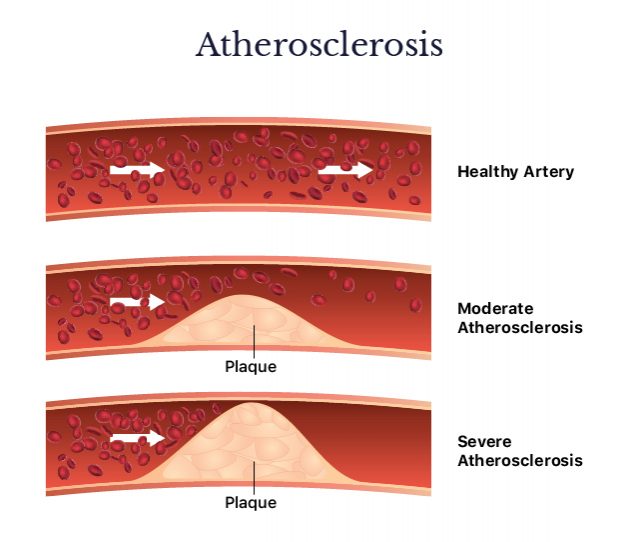
Heart Defects
Sometimes heart defects block or obstruct the flow of blood to the heart. These blockages occur in the valves, arteries or veins, a condition referred to as stenosis.
“You can be perfectly healthy with a bicuspid aortic valve that develops valvular problems. That’s strictly genetic,” said Noorchashm.
Congenital heart defects are diagnosed at birth. Newborns with serious heart defects may have grayish or blue skin; swelling in the legs, abdomen or around the eyes; and shortness of breath.
Some older children or adults may experience symptoms of heart defects later in life. These symptoms include shortness of breath, weakness, fatigue with exercise and swelling in the ankles, hands or feet.
Congestive Heart Failure
Heart failure doesn’t necessarily mean the heart has stopped or that a person is going to die. Rather, it means the heart isn’t squeezing as well as it should and, as a result, isn’t pumping enough blood to parts of the body.
This condition occurs gradually. Diabetes, heart defects, high blood pressure and prior heart attacks can put a person at risk for heart failure.
- Confusion, trouble concentrating or decreased alertness
- Coughing up pink or bloody phlegm
- Edema (swelling) in the abdomen, feet, ankles or legs
- Fatigue or tiredness
- Fluid buildup in the lungs
- Nausea and loss of appetite
- Persistent cough or wheezing
- Rapid or irregular heart beat
- Rapid weight gain
- Shortness of breath
- Sleep apnea
Cardiomyopathy
Cardiomyopathy is a disease that causes the heart to pump harder than it should, leading to an enlarged heart that is thicker and more rigid than normal. Heart attacks, high blood pressure or infections may lead to cardiomyopathy.
People with cardiomyopathy may also suffer heart failure, abnormal heart rhythms, heart valve problems and heart attacks.
- Breathlessness, even when resting
- Chest pain, discomfort or pressure
- Coughing when lying down
- Dizziness, lightheadedness and fainting
- Fatigue
- Irregular heart beat or heart murmurs (unusual sounding heartbeats)
- Swelling of the abdomen, legs, ankles and feet
What Increases Risk?
Several factors put a person at risk of developing heart disease. Some factors, like diet or smoking, are in our control. Others, such as family history, are not.
“I would say that there are intrinsic risk factors that have to do with the biology of the heart itself or…to patients’ susceptibility to things like high cholesterol, high blood pressure and diabetes,” said Noorchashm. “Then there are environmental things such as smoking, such as excessive intake of high-carbohydrate and [high-] fat foods that lead to obesity. Most of us sort of have interplay between intrinsic genetics and environment that leads to heart disease.”
The CDC breaks these factors down into three groups: conditions, behavior and family history (or genetics). Certain medications may also increase heart disease risk.
“Most of us sort of have interplay between intrinsic genetics and environment that leads to heart disease.”
Conditions
Certain health conditions can increase the risk of heart disease. These include high blood pressure, high cholesterol, diabetes and obesity.
Excessive stress can also negatively affect your blood pressure and cholesterol and damage your arteries, according to Cleveland Clinic.
In addition, poor mental health can contribute to poor heart health.
A study by Dr. Marc De Hert and colleagues at the KU Leuven University Psychiatric Centre in Belgium found that people with severe mental illnesses such as major depressive disorder, schizophrenia and bipolar disorder have an increased risk of coronary heart disease.
Behavior
Behavior encompasses the lifestyle choices people make that increase their risk of heart disease. Adopting healthy behaviors can help lower heart disease risk.
Unhealthy habits include eating foods high in saturated fats, trans fat, salt or cholesterol; not getting enough physical activity; drinking too much alcohol; and smoking (including exposure to secondhand smoke).
“There are intrinsic risk factors that have to do with the biology of the heart itself or to patients’ susceptibility to things like high cholesterol, high blood pressure and diabetes.”
Family History, Age and Ethnicity
Family history, age and ethnicity are risk factors that people cannot control. For example, some individuals are genetically predisposed to have high blood pressure, high cholesterol or other conditions that affect heart health.
Certified nutritionist Rebecca Montrone has done research into some hereditary risks. According to Montrone, mutations in the MTHFR C677T gene along with high levels of homocysteine — a common amino acid in the blood — can lead to inflammation and elevated levels of blood coagulation that may narrow the arteries or cause blood clots.
Families also may share environmental factors that contribute to heart disease such as an unhealthy diet or lack of physical activity. Lifestyle factors such as smoking or excessive alcohol consumption can amplify these risks.
Risk also increases as people age.
Medications
Some prescription drugs may increase heart disease risk. These drugs are used to treat diseases such as diabetes, depression, and cancer. Other drugs may also cause effects that increase cardiovascular risk. If you are at high risk for heart disease, ask your doctor or pharmacist whether medications you take or are prescribed can affect your risk.

Heart Disease in Men and Women
Heart disease is the number one killer of men and women in the United States, though slightly more men die from it.
Because of the misconception that heart disease only affects men, only about 56 percent of women know it’s their number one killer, too, according to the CDC.
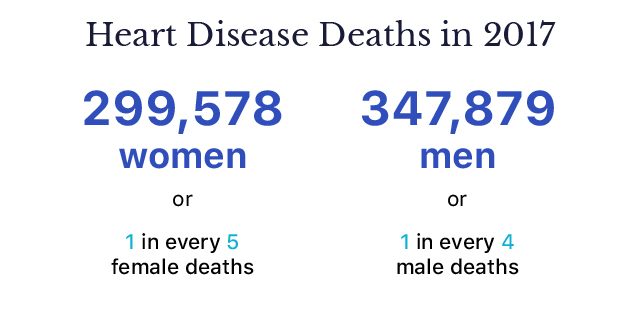
Source: Centers for Disease Control and Prevention
“I think generally it’s agreed that women are less susceptible [to heart disease] because of the hormonal makeup of women…although the difference is not a huge difference,” said Noorchashm. “The same risk factors are operational.”
Heart attack symptoms may manifest differently in men and women. Women are more likely to have shortness of breath and nausea during a heart attack, and they are also more likely to die.
Heart Problems More Likely to Affect Women
While more men may die of heart disease, women are more susceptible to certain types of disease including angina, cardiac syndrome X, and broken heart syndrome.
Angina or chest pain affects about 4 million women in the United States. Women are more likely than men to experience stable angina and variant angina.
Cardiac syndrome X happens when people with healthy, unblocked arteries feel chest pain and artery spasms. Hormonal changes after menopause make women more likely to have heart problems.
Broken heart syndrome is also called stress-induced cardiomyopathy. While researchers don’t know its exact cause, extreme stress or intense grief, surprise, or anger can trigger symptoms. It may be misdiagnosed as a heart attack, though there are no blocked arteries.

Common Treatments
So far there is no cure for heart disease, according to Cleveland Clinic. But providers can improve a patient’s health and try to prevent serious problems like heart attacks and strokes.
Common treatments for heart disease include lifestyle changes, medication, and, in serious cases, surgery.
Most experts agree that getting more physical activity and eating a diet rich in fruits and vegetables and low in saturated fat reduces the risk of heart disease and keeps it from getting worse.
Some patients may need medication to help control risks like high blood pressure and cholesterol if diet and exercise are not enough. For example, controlling high blood pressure with drugs like valsartan and maintaining healthy cholesterol levels with Lipitor or other statins may partially reverse plaque in the arteries.
Patients with advanced heart disease may need surgery. Bypass surgery can help open blocked blood vessels and repair and replace diseased valves. Some patients with heavily damaged hearts may require heart transplants.
“Once the surgery is performed successfully, you want to prevent recurrent disease. At that point, you collaborate with a cardiologist and you risk-manage the patient. Keep their cholesterol down, keep their blood pressure down,” said Noorchashm.
Studies on Diet and Supplements
In addition to the usual medications, some nutritionists are looking into certain foods and supplements that might prevent heart disease.
Rebecca Montrone is a certified nutritionist who has helped people lower their heart disease risk. She recommends cutting out sugar and processed foods as well as eating plenty of vegetables.
But some of her findings are controversial when it comes to fat, low-density lipoprotein (LDL), sometimes called “bad” cholesterol, and high-density-lipoprotein (HDL), or “good” cholesterol. Most guidelines discourage saturated fat consumption, but Montrone advises people to eat more of it.
“Contrary to the usual advice, [eat] plenty of good quality saturated fats [such as] butter, coconut oil, animal lard, and fatty meats,” Montrone told Drugwatch in an email.

She recommends taking 500 to 1000 mg of niacin daily to lower LDL.
Increasing LDL particle size can also help lower heart disease risk, Montrone said. Eating saturated fats “changes their gnarly, inflammatory, arterial-damaging size into white fluffy clouds that do not damage the arteries that then provoke the deposition of plaque.” She also stated that “statin drugs do not lower small particle LDL, can increase triglycerides, and can lower HDL.”
Some studies may support Montrone’s recommendations about fat consumption and diet. For example, one study by Dr. Hussein M. Dashti and fellow researchers found that a high-fat, long-term ketogenic diet lowered triglycerides, LDL, and blood glucose in obese patients.
Another study led by Dr. Joyce A. Nettleton and researchers in the Netherlands found that saturated fat didn’t actually increase the risk of cardiovascular problems, though replacing saturated fat with polyunsaturated fat reduced risk by 17 percent.
An older study made famous by the documentary Forks Over Knives makes the argument for reducing the consumption of fat and animal products.
The 1995 study by Dr. Caldwell B. Esselstyn, Jr., and colleagues at the Cleveland Clinic studied the effects of a low-fat diet (with no animal products except for skim milk and low-fat yogurt) and statins on people who had prior heart attacks, strokes, and bypass surgeries.
Researchers found that the treatment prevented the majority of study participants from having additional coronary events. Some participants even had a reversal of artery damage.
Check with your doctor before changing your diet or taking any supplements.

What Can You Do to Lower Risk?
Preventing heart disease remains the number one way to avoid complications such as heart attacks, strokes, and artery disease. The CDC has some tips for lowering heart disease risk.
- Control blood pressure
- Eat a healthy diet
- Get enough sleep
- Exercise
- Quit smoking
- Keep cholesterol and triglyceride levels normal
- Limit alcohol
- Manage diabetes
- Manage stress
- Stay at a healthy weight
Noorchashm recommends that people stay proactive with their health.
“I think the most important piece of advice to give people is to make sure that they have a good handle on their cardiac risk factors in consultation with their primary medical provider,” said Noorchashm, “and if they are at a high risk, to make sure that a cardiologist is sort of guiding them.”